Today, on International Day of the Midwife (May 5), midwives share what it’s like working through a pandemic.
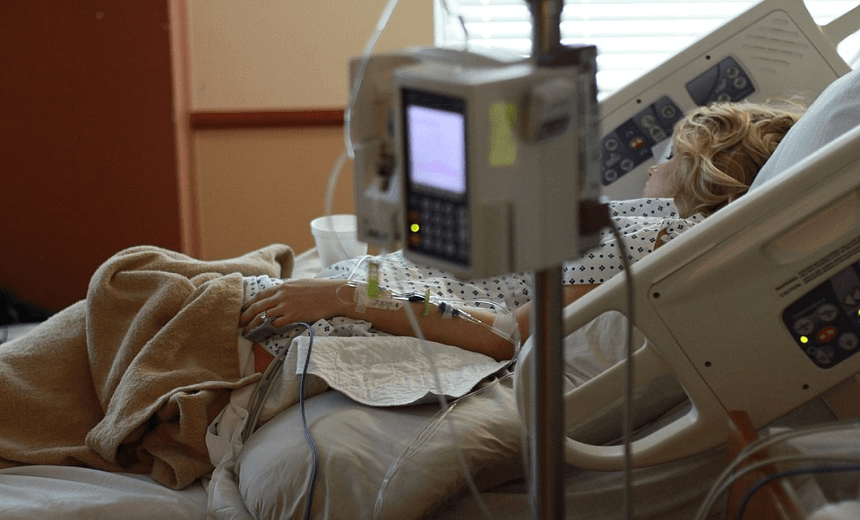
As you read this new lives will be delivered into the world. Not just new babies, but new parents too. For those women birthing, this might be the most powerful and strong, scared and overwhelmed, vulnerable and hopeful they’ve ever felt. They’ll remember these days for the rest of their lives. About 6700 babies have been born during alert levels four and three in New Zealand. No matter what the state of the world, babies are always born.
Midwives hold many lives in their hands – not just of baby, but mother too. The role has always been an enormous one, and over recent years the workload has only increased. In New Zealand in 2020, the international year of the midwife, some maternity carers say it feels untenable.
Midwives were meant to catch a long awaited break this year. The hope was that with pay equity midwives would have a sustainable funding model that finally acknowledged the crucial role they play and the huge workload they carry in caring for all communities.
And then Covid-19 happened. The challenges have been immense for many midwives.
The pressure is particularly intense in the area covered by Southern District Health Board, midwives say. Due to safety concerns, birthing mothers in Queenstown were recently moved out of the maternity unit at Lakes District Hospital and across the road into what had been a dental clinic. The clinic had no functioning shower, so a portable one was erected by the side of the road. The shower barely worked, one midwife told Stuff. “Water just dribbles out, there is no heating, there is no privacy.”
Now, because of the showering issue at the clinic, some midwives are instead using a local hotel for birthing, at a cost to mothers of $195 a day.
“[The hotel] has no hospital facilities or doctors nearby or staff midwives overnight like the dental clinic does. Women already feel vulnerable birthing two and a half hours away from the nearest base hospital. Covid-19 just exacerbated issues that were already here,” midwife Holly* told The Spinoff.
Holly says Southern DHB made decisions about moving the unit without consulting local midwives. “And then it’s up to us to front this to our women and apologise for it.”
“The one good thing that has come out of the move is something that has been fought for, for almost a decade, and that’s a birth pool is being installed in the birth unit. However, this also delays our return to the unit. This was again decided upon without consulting midwives and I’d rather use postnatal rooms and be in the main (hospital) building with access to safe, warm showers and doctors in ED only a corridor away.
“The saddest thing is Southern DHB recently closed a beautiful and perfectly set-up birth unit half an hour away in Lumsden. Why couldn’t we use that as our interim birth unit instead of a place where women have to shower by the road?”
In a statement, Southern DHB associate general manager Debi Lawry said the temporary relocation of the birthing unit was a safety measure as part of the Covid-19 response. “Whilst not purpose-built, the building has provided a safe environment, away from the potential exposure to Covid-19 positive cases, for mothers and babies to receive good, safe clinical midwifery care.
“The temporary facility does not have a permanent shower, although some alternative, less accessible options have been provided. This has not appeared to be such an issue for the women, as they understood the constraints in this Covid-19 dominated world. They identified they wanted skilled midwifery care in a safe environment.”
The Spinoff spoke to other midwives around the country about how Covid-19 has affected their jobs. Kate* a midwife working in Bay of Plenty, says her immediate response was fear and confusion. “Immediately I had women texting me asking me what this meant for them. But I had no idea what it meant. Nobody did, but somehow I was expected to know.”
In the days that followed Kate worried for her family – her father is sick and her daughter has an auto immune disease.
“I was scared for myself and I was scared for my women. I had no idea how I was meant to work and social distance and keep myself and others safe. How do I do that when I am in everyone’s bubble?“
Jumping from bubble to bubble is frightening, Kate says, and she feels a huge responsibility – not only to mothers and babies, but to also keep her own family safe. Between texts and phone calls she describes as “endless”, she has to keep calm and prioritise care.
Clinics and post-natal appointments had to completely change their operations due to social distancing, she says. “I have women cry in my clinic, new mums needing a reassuring hug and I can’t. I’ve not cuddled a baby for too long now.
“It breaks our hearts. The lovely part of our job, the bit that people say ‘oh it must be so lovely doing that’, it’s gone. For now. It’s been really, really hard. And I also miss my people. I can’t wait to hug and see my dad.”
There’s a part of the job of midwife that goes beyond practical birth care. “The hard stuff”, Kate calls it.
“The hard discussions, miscarriage, domestic violence, social issues, emergencies and the long, long, long days and nights, plus all the paperwork. I easily worked 32 hours this last weekend, much of it unpaid.”
Jane*, a midwife in the Hawke’s Bay region, says constantly having to explain changes to her women, when she’s still trying to get information herself, has been hard. “We’re trying to explain how the scan, previously deemed as necessary by an obstetrician, can now suddenly wait, or the blood test that you ordered is no longer available as the lab has now been directed to do Covid swabs.”
An increase in cleaning, hand washing and sanitising, both during and between visits is as crucial as it is time-consuming. PPE hasn’t always been available, Jane says. Friends, family, and clients have stepped in to provide it.
In her region there have been 22 home births in the last month, she says.
“Parents are choosing this option rather than expand their bubble too far, ensuring they can be together for all of the labour and birth. As wonderful as it is to attend a home birth, I have to source and pay for the equipment used there – this is time-consuming and can be expensive.”
Mae, a midwife working in the South Island, says she’s found midwifery during Covid-19 an overwhelming experience. She works at a primary maternity unit, supporting parents through labour and their first days as parents.
“We are a ‘green zone’ which means that although only people with no risk factors for Covid-19 could come to the unit, we still have had to practise physical distancing,” she says.
“Midwives get in there. It’s in our DNA. It’s impossible to do hands-on breastfeeding support from a distance. And sharing the exuberance of triumphant births with women and their support person while in full PPE doesn’t come easily.”
Still, Mae describes her work as “amazing” and “soul-nourishing”.
Today, more babies will be born. Midwives will be there. This pandemic has shown exactly what most parents already knew: midwives are an essential workforce in Aotearoa. Not just today on the Day of the Midwife, but every day.