Covid has highlighted South Auckland’s potential vulnerability to a health crisis, so what are our politicians promising to do about the region’s ongoing problems?
Updated with statistics minister James Shaw’s comments.
Mary* is a GP in South Auckland.
She’s on the frontline, helping those with often complex health issues in one of New Zealand’s most vulnerable regions, and she is growing more and more frustrated with the support for her patients from Counties Manukau DHB, particularly through Middlemore Hospital.
“There are so many examples of people falling through the gaps and it’s because they are probably overworked in the hospital,” says Mary. “It seems we’re just providing band aid solutions – and we’re not fixing the root causes of the issue. I have no idea what kind of wrap-around service they have there, but there seems to be a disconnect between us and the hospital.”
She raises a number of examples, including a situation where a patient needed to be tested for cancer but due to delays he had to wait 13 days for a diagnosis after the initial appointment. She says this delay may have resulted in the cancer getting worse.
“He wasn’t really listened to,” she says. “He had delays in getting extra scans, delays in getting his case reviewed and then the specialists were delayed. It’s unacceptable in the sense that there was a high chance he had cancer, and this is an aggressive cancer – if he had been diagnosed within the first week, would it have progressed as much? That’s a question we just don’t know the answer to.”
She gives another example of a patient whose heart issues were not picked up early enough and as a result, treating him is proving difficult. She says communication breakdown is often part of the problem.
“The language barrier is a huge thing,” she says.
“A lot of diagnoses come from understanding family history – so if you don’t have an interpreter there, you’re not going to fill in the gaps and it’s going to be incorrect and it’s just too simplistic to blame the individual.”
Steve* is another South Auckland-based GP, who has also worked at Middlemore, and he shares Mary’s concerns.
“There was a Pacific support team who would provide Pacific patients with support and help navigating the hospital system – but apparently the service was downsized. In an environment where people are unwell and suffering and the way things work are unfamiliar or even hostile, this was extremely disappointing from a clinical perspective, considering how important that support is for patients getting the best health outcomes from their stay in hospital.”
He believes the DHB is being forced into choosing between clinical services and the wrap-around support that can ensure clinical services are more effective.
“It kind of showed that when the financial shove comes, it’s some of the less clinical services that get pushed out, but this support service is arguably one of the most important with regards to how the hospital engages with Pacific patients.”
As pointed out by Counties Manukau Health’s director of population health Dr Gary Jackson in an earlier interview on this subject, census undercounts of South Auckland’s Pacific population are resulting in the DHB missing out on much-needed operational funding.
“It’s incredibly frustrating,” he said in our previous article. “We’re a DHB which is dealing with the largest number of Pasifika people, the second-largest number of Māori people, the highest number of people living in the most deprived areas, and yet we’re the DHB that’s getting penalised by the population count. We do a reasonable job at being efficient at allocating money, but we’re going to be running a $30 million deficit this year, which is essentially this [missing] money.”
So how will the next government deal with the inequities being experienced by those in South Auckland?
National Party health spokesperson and Whangārei electorate MP Dr Shane Reti says it starts by ensuring the next census isn’t botched like the last one.
“It just seems like they [the government] were distracted, they took their eye off the ball … they didn’t follow the methodology, and they were late to react when they realised it wasn’t working, but the implications of this are wide ranging. Northland, for example, doesn’t get the health funding that it truly should have. The census is a baseline for so much government funding that if you get that wrong, you fundamentally miss out on funding.
“[For Census 2023] I would be making sure we wouldn’t be making the same mistakes as the 2018 census. We would project manage this more closely, monitor it more closely, and react more quickly and have other portfolio holders keeping an eye on it.”
To address inequities, National is also promising to fund a “primary-care navigator” for every general practice to boost frontline health services’ capacity and require DHBs to annually report against a Māori health strategy.
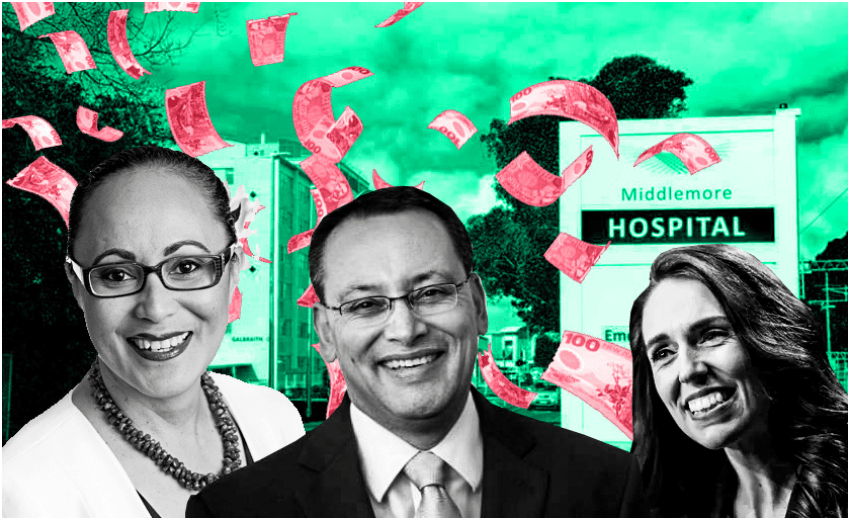
Labour Party leader Jacinda Ardern says, if re-elected, her party will deal with how DHBs are funded, taking into account regions with high levels of deprivation.
“I haven’t received anything specific to the information that Counties Manukau has raised,” she says.
“But more generally when it comes to health funding, we have had an ambition and a concern that currently the way we calculate the support for our DHBs is often very heavily weighted on population growth and it doesn’t necessarily take into account some of those health disparities. So in the work we are doing around health sector reform, that is something I hope we will be able to address.”
Labour’s Jenny Salesa is the associate health minister and electorate MP where Middlemore Hospital is located. She says part of her government’s efforts is the $17 million Ola Manuia: Pacific Health and Wellbeing Action Plan 2020-2025, announced earlier this year, which aims to develop new and innovative methods to improve Pacific health.
“Population-based funding is not an issue that has arisen just over the last three years,” she says.
“Improving the health and wellbeing of all Pacific people in New Zealand has been a priority of mine, and of this government. Alongside [Ola Manuia], inequalities and funding distribution will be considered during the implementation of the Simpson report into the health and disability sector.”
And when it comes to the next census in 2023, statistics minister James Shaw says there will will be better, more targeted engagement with population groups that were undercounted in the 2018 Census.
“Stats NZ has $210 million available to run the 2023 Census – a two thirds increase on the total cost of the 2018 Census,” he says. “This funding boost means there will be more boots on the ground for the census operation and more paper based forms available from the outset. On top of this, Stats NZ is working hard to design and execute targeted engagement strategies with communities, including the Pacific community, and the South Auckland community.”
This extra funding will also go towards implementation of a Pacific engagement strategy and see a 150% increase in door-knocking staff.
Auckland councillor Fa’anana Efeso Collins is also the chairperson of Ōtara Health, which has been helping run a food bank and testing station over the last six months. He says while South Aucklanders might feel a little bit cynical about the different proposals being suggested to turn around the region’s dire health statistics, he believes Covid has highlighted ways the region is also starting to take a greater lead in resolving its own issues.
“What this year has shown us is that our Pacific community and South Aucklanders in general are able to step up time and time again,” he says. “Our people got tested in large numbers and so many of our local organisations mobilised to provide food support during the two lockdowns. I think we can see there’s a growing community resilience that hopefully can translate into ensuring better health outcomes for our community into the future.”
Comment was sought from the Counties Manukau District Health Board, but a spokesperson said the DHB did not wish to comment at this time.
*Mary and Steve are not the real names of the doctors mentioned in this article.